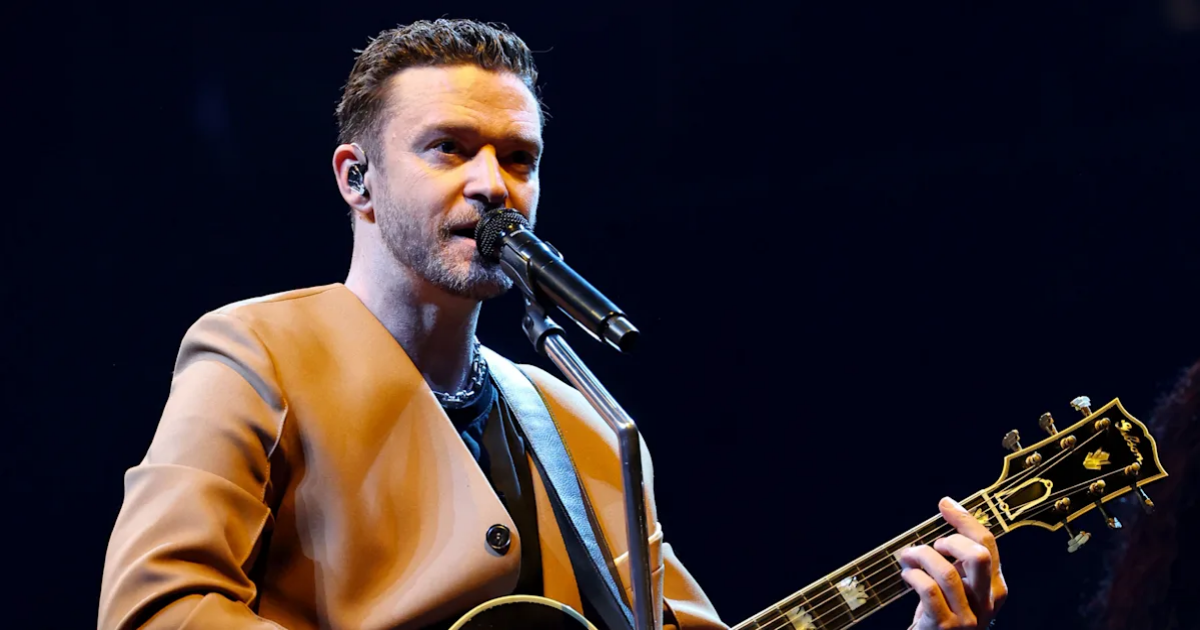
Justin Timberlake says he was recently diagnosed with Lyme disease, the tick-borne illness that affects hundreds of thousands of people each year — and is on the rise.
“I’ve been battling some health issues, and was diagnosed with Lyme disease,” Timberlake wrote in a post on Instagram Thursday. “If you’ve experienced this disease or know someone who has — then you’re aware: living with this can be relentlessly debilitating, both mentally and physically.”
Timberlake recently wrapped up a two-year, 41-stop world tour.
“When I first got the diagnosis I was shocked for sure,” his post continued. “But, at least I could understand why I would be onstage and in a massive amount of nerve pain or, just feeling crazy fatigue or sickness.”
Some of Timberlake’s recent performances were criticized by fans for being low-energy and lackluster.
The singer said he considered halting his tour but decided that “the joy that performing brings me far outweighs the fleeting stress my body was feeling.”
By sharing his Lyme diagnosis, Timberlake added, “I’d like to do my part to help others experiencing this disease.”
Over 89,000 cases of Lyme disease in the United States were reported to the Centers for Disease Control and Prevention in 2023, an increase of more than 40% in the number of cases that were reported in 2022. But the CDC says that other estimates suggest far more people — approximately 476,000, per one 2021 study — may be diagnosed and treated for Lyme in the U.S. each year.
We spoke with experts who explained how Lyme disease is contracted, its symptoms, which areas are hot spots and what you can do to stay safe.
What is Lyme disease and how is it contracted?
The Northeast, the Upper Midwest and the West Coast are hot spots for ticks. (Getty Images)
Lyme disease is an infection caused by spiral-shaped bacteria known as spirochete, the most common ones in the U.S. being Borrelia burgdorferi and Borrelia mayonii, Dr. Bobbi Pritt, a Mayo Clinic microbiologist, pathologist and Lyme disease expert, tells Yahoo Life. “Most people get it after being bitten by an infected black-legged tick, also called a deer tick,” Pritt adds. “These ticks become infected with the Lyme bacterium by biting an infected rodent, bird or other animal.”
Symptoms can show up within three to 30 days after a tick bite. Most people develop a target-shaped rash at the site of the tick bite and flu-like symptoms including fever, chills, fatigue, headache, lack of appetite, neck stiffness, swollen lymph nodes and muscle and joint pain, explains Pritt. However, some people don’t get a rash at all, “or fail to notice it if it’s on the back, scalp or other hard-to-see area,” she says.
How is Lyme disease treated?
If left untreated, the infection can spread and symptoms may worsen, resulting in arthritis, bone and joint pain, additional rashes, inflammation of the brain and spinal cord and facial palsy (one-sided facial droop), explains Pritt. “Involvement of the nerves can cause shooting pains or numbness in the hands and feet,” she says. Although not common, “involvement of the heart can lead to inflammation and rarely death.”
Treatment for Lyme disease varies depending on the case and symptoms, but almost always includes a course of oral or intravenous antibiotics, per the CDC. Even with treatment, though, 5% to 10% of infected individuals have persistent symptoms including fatigue, body aches and brain fog, Pritt says. “It can take months for these symptoms to go away,” she says. “Therefore, it is important to take steps to prevent Lyme disease whenever possible.”
What are the hot spots for Lyme disease?
Hot spots for Lyme disease are the Northeast, Upper Midwest and West Coast, as evidenced by the CDC’s Lyme disease map. Not surprisingly, vast areas of brush and trees cover these areas, where hiking and outdoor recreation are popular. “In the past, Lyme disease appeared to be limited to specific regions of the U.S.,” says Dr. Mark Loafman, a family physician with Cook County Health in Illinois. But anywhere with dense forestation presents risk.
Climate change could also be making things worse, adds Loafman, as deer ticks thrive in warm environments. Freezing temperatures typically control their population, according to NASA, but as winter temperatures rise in the northern U.S. and Canada, so does Lyme disease risk.
5 ways to protect yourself from Lyme disease
There are steps you can take to lower your risk of tick bites and Lyme disease, according to Loafman and Pritt.
- Avoid hot spots. Using the CDC’s map as a guide, it’s wise to avoid Lyme disease hot spots, especially in warmer months. If that’s not possible, and you spend extensive time outside in those regions, Pritt recommends avoiding dense vegetation like tall grasses and leaf litter, environments in which ticks thrive.
- Wear protective clothing and tick repellent. During outdoor activities, it’s crucial to wear clothing that covers your skin — even when it’s hot. “Tucking your pants into your socks can be an easy and effective way to keep ticks from biting your legs,” Pritt says. She also recommends using tick repellents such as Deet, Picaridin and oil of lemon or eucalyptus. For an added layer of protection, you can treat clothes and gear with the insecticide permethrin.
- Complete thorough tick checks often. Especially after being outdoors, it’s important to scan the entire body for tick bites. Loafman notes that deer ticks are tiny, “so the skin inspection must be thorough and close,” he says. The insects like to burrow snugly against the skin, he adds, which makes the groin, armpits, inner elbows, waist band and sockline common areas for them to hide.
- If you find a tick, remove it immediately. “Ticks take their time setting up shop to feed on your blood, so it generally takes 36 to 48 hours to transmit infection,” says Loafman. That means the sooner you remove a tick, the less likely you are to get sick. Still, Loafman advises doing so carefully and with caution — Pritt suggests using tweezers — because crushing or injuring the tick can cause injection of its saliva and make things worse.
- Save the tick and see your doctor as soon as possible. After tick removal is complete, Loafman recommends putting it in a sealable plastic bag and taking it to your primary care provider, whom you should see as soon as possible. “Depending on the circumstances, they may want to see the tick to help determine the risk,” he says. Most important, if you suspect you were bitten — whether or not you found a tick — it’s important to see a doctor. “Treatment can help even if days or weeks have passed,” Loafman says.